Peripheral artery disease (PAD) is a serious yet often overlooked cardiovascular condition that affects blood flow to the limbs, most commonly the legs. It develops gradually and may go unnoticed in its early stages, increasing the risk of complications such as heart attack and stroke. Understanding the symptoms and causes of PAD is essential for early diagnosis, timely treatment, and preventing long-term damage to blood vessels.
What Is Peripheral Artery Disease (PAD)?
Peripheral artery disease occurs when arteries that supply blood to the arms or legs become narrowed or blocked due to plaque buildup. This process, known as atherosclerosis, reduces oxygen-rich blood flow to muscles and tissues. As a result, everyday activities like walking can become painful. PAD is a sign of widespread vascular disease and often indicates underlying heart or brain artery problems.
How Blood Flow Is Affected in PAD
Healthy arteries allow blood to flow smoothly throughout the body. In PAD, fatty deposits accumulate along artery walls, making them stiff and narrow. When muscles require more oxygen—such as during walking or climbing stairs—the restricted blood flow cannot meet the demand. This leads to muscle fatigue, cramping, and discomfort. Over time, reduced circulation can impair wound healing and tissue health.
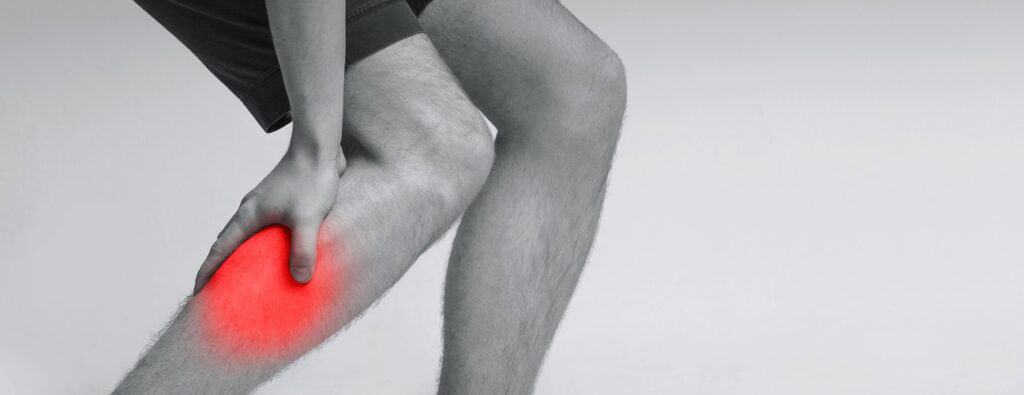
Early Symptoms of Peripheral Artery Disease
Many people with PAD experience mild or no symptoms initially. As the disease progresses, the most common early symptom is leg pain during physical activity, known as intermittent claudication. This pain typically affects the calves, thighs, or hips and eases with rest. Other early signs may include leg weakness, numbness, tingling, or a feeling of heaviness during movement.
Advanced Symptoms and Warning Signs
In advanced stages, PAD symptoms become more severe and persistent. Pain may occur even at rest, particularly at night. The skin on the legs or feet may appear pale, bluish, or shiny, and hair growth may slow or stop. Non-healing sores, ulcers, or infections on the feet are serious warning signs and indicate critically reduced blood supply requiring urgent medical attention.
Impact of PAD on Daily Life
Peripheral artery disease can significantly affect mobility and quality of life. Walking short distances may become difficult, limiting independence and physical activity. Reduced activity can worsen cardiovascular health, leading to weight gain and poor blood sugar control. Emotional effects such as frustration, anxiety, and fear of pain are common, highlighting the importance of early management and lifestyle adjustments.
Primary Causes of Peripheral Artery Disease
The primary cause of PAD is atherosclerosis, a condition in which cholesterol and fatty substances build up in the arteries. Smoking is the strongest risk factor, as it damages blood vessels and accelerates plaque formation. Other major causes include diabetes, high blood pressure, and high cholesterol levels, all of which contribute to artery narrowing over time.
Risk Factors That Increase PAD Development
Several factors increase the likelihood of developing PAD. Age over 50, family history of cardiovascular disease, obesity, and a sedentary lifestyle are significant contributors. Diabetes plays a major role by damaging blood vessels and nerves. Chronic kidney disease and prolonged stress also increase vascular inflammation, making arteries more vulnerable to blockage.
Complications Associated With Untreated PAD
If left untreated, PAD can lead to serious complications. Poor circulation increases the risk of infections, gangrene, and in severe cases, limb amputation. PAD is also a strong indicator of systemic atherosclerosis, raising the risk of heart attack and stroke. Early diagnosis and proper cardiovascular care are critical to preventing these life-threatening outcomes.
How PAD Is Diagnosed and Evaluated
Diagnosis of PAD involves a detailed medical history and physical examination. Doctors may check pulses in the legs and perform tests such as the ankle-brachial index (ABI) to compare blood pressure in the arms and legs. Imaging studies like Doppler ultrasound or angiography help assess blood flow and determine disease severity, guiding treatment decisions.
Book Appointment With Best Cardiologist in Karachi via InstaCare
If you experience leg pain, numbness, or poor wound healing, it is essential to consult a heart and vascular specialist. Through InstaCare, you can easily book an appointment with the best cardiologist in Karachi for expert evaluation and personalized treatment. InstaCare connects you with trusted cardiologists offering advanced diagnostic tools and comprehensive care for PAD and related heart conditions.
Conclusion
Peripheral artery disease is a progressive condition that affects circulation and overall cardiovascular health. Recognizing symptoms early and understanding the underlying causes can prevent severe complications. With timely diagnosis, lifestyle changes, and professional medical care, PAD can be effectively managed. Consulting an experienced cardiologist ensures the best outcomes and long-term vascular health.
Frequently Asked Questions (FAQs)
- Is peripheral artery disease the same as heart disease?
PAD affects arteries outside the heart, mainly in the legs, but it is closely linked to heart disease and increases cardiovascular risk. - Can PAD be reversed?
While artery damage cannot be fully reversed, lifestyle changes, medications, and medical procedures can slow progression and relieve symptoms. - Is leg pain always a sign of PAD?
No, leg pain can have many causes, but pain during walking that improves with rest is a common PAD symptom and should be evaluated. - Does PAD affect both legs?
PAD can affect one or both legs, depending on where artery blockages are present. - When should I see a cardiologist for PAD symptoms?
You should consult a cardiologist if you have persistent leg pain, numbness, non-healing wounds, or known risk factors like diabetes or smoking.